The Relationship Between Osteoporosis and Cancer
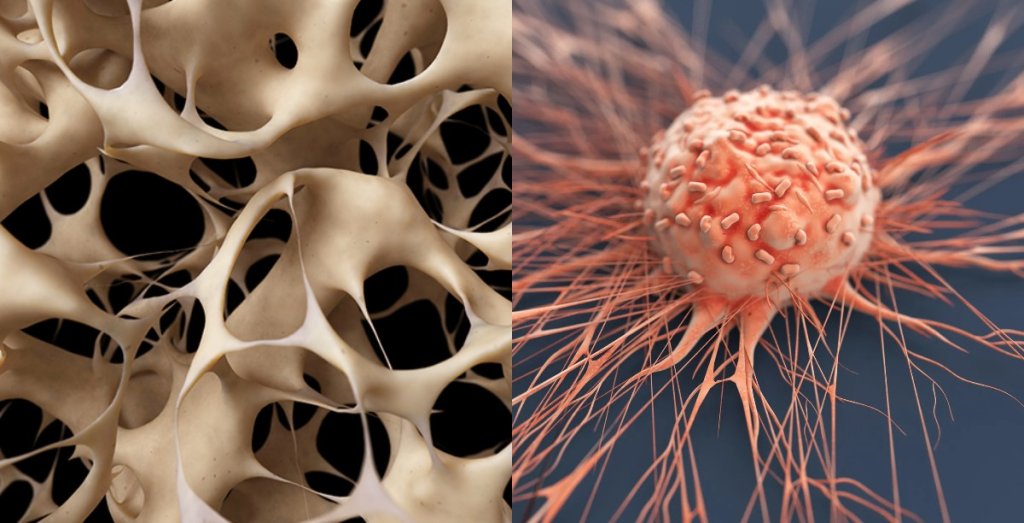
Thinning bones in osteoporosis can make them brittle and break. In cancer, uncontrolled cell growth, inflammation, and certain types of cancer treatment can also negatively affect bones, making them more vulnerable to fractures. What does this mean for bone health?
This article explores the relationship between osteoporosis and cancer and what it means when going through certain cancer treatments. You will also learn how to manage both in the most effective way, one on one.
The Link Between Osteoporosis and Cancer
If you have osteoporosis, your health care professional will monitor your bone health and check your bone mineral density for any signs of weakening.
One of the associations in the middle of osteoporosis and cancer is aging in general. Aging is certainly associated with osteoporosis. Cancer is also more likely to occur in older individuals.
As people of a random sex age, sex hormone levels tend to drop. The sex hormone estrogen protects against bone loss.
Estrogen levels for menstruating people drop as they approach menopause (when the monthly ovulation cycle stops). Estrogen levels can drop as much as 90% at menopause. This drop in estrogen levels causes bone thinning.
A number of studies have shown that bone density is also linked to decreased availability of sex hormones in individuals designated as male at birth. They become increasingly attached to a protein that prevents them from being active. This reduction averaged 47% for estrogen and 64% for testosterone. Less active estrogen means decreased bone mineral density.
Cancer can also cause bone loss. In cancer that has not metastasized (spread beyond its original site), increased inflammation in both the cancer site and the body can lead to bone loss. Bones are also a common site of metastasis, affecting the skeleton.
While some forms of cancer treatment can improve survival, they can also weaken bones. Cancer treatments may aim to reduce estrogen or testosterone to slow cancer growth (especially when treating breast or prostate cancer). Blocking these protective hormones can cause bone weakening.
Cancer treatments that may increase the risk of osteoporosis include:
- Aromatase inhibitors such as Femara (letrozole), Arimidex (anastrozole), Aromasin (exemestane)
- Gonadotropin-releasing hormone agonists such as Zoladex (goserelin) and Lupron (leuprolide)
- Surgical removal of the ovaries or testicles
- Androgen deprivation therapy such as Casodex (bicalutamide), Eulexin (flutamide), Nilandron (nilutamide)
- Steroids such as prednisone and cortisone
- some chemotherapy drugs
- Medicines that suppress the immune system, such as methotrexate
risks
Cancer patients may find that they are not just at increased risk of osteoporosis from the cancer itself. Types of cancer that can lead to bone loss include:
- bone cancer
- breast cancer
- Prostate cancer
- Lung cancer
- Multiple myeloma (cancer of plasma cells)
Bones and ones in particular are at risk.
The specific treatment you need to manage your cancer may also be a factor. When bone loss occurs due to cancer treatment, it can be more than seven times that of classical aging. It is typically faster and more severe.
If this condition actually affects your bones, cancer treatment can exacerbate osteoporosis. It is another risk factor that you need to weigh.
Cancer Treatment and Management of Osteoporosis
or directly increasing the risk of osteoporosis may affect how your cancer is managed. Your oncologist (a doctor who specializes in treating cancer) will want to weigh the possibility of your bones weakening and potentially developing fractures.
Some risk factors not related to cancer include:
- Your age
- If you are postmenopausal
- Whether you are a smoker
- Whether you drink alcohol
- If you have had other fractures as an adult
- Whether your body is producing enough sex hormones
- if you are weak
- If you have a family history of hip fracture
If you’ve been diagnosed with cancer and have at least one other risk factor for osteoporosis, you’ll likely be asked to do a bone mineral density test. In cases where your oncologist has prescribed an anti-cancer drug known to cause bone loss, this test should be repeated at least every two years, if not earlier.
If you have osteoporosis or are at high risk of developing osteoporosis, you may be given bone-modifying drugs to help reduce the risk of fractures. These include bisphosphonates. Like Zometa (zoledronic acid).
As a rule, hormone replacement therapies (such as estrogen replacement therapy) that are known to protect the bone will be avoided if you have hormone-sensitive cancer as it stimulates the growth of the cancer.
Prevention
Being diagnosed does not mean that you are destined to develop osteoporosis. To help prevent osteoporosis from occurring along with a random cancer diagnosis, you will likely be advised to do the following:
- Increase the amount of calcium and vitamin D you consume. You will probably be recommended to consume at least 1,000–1,200 milligrams of calcium per day and 800–1,000 international units (IU) of vitamin D per day.
- Quit smoking as it can affect bone quality and increase the risk of fractures.
- Stop drinking alcohol, which can affect your balance and otherwise cause falls.
- Train to improve balance, strength and flexibility and reduce the chance of falling.
Summary
Osteoporosis naturally occurs with age, but it can also be brought on by cancer. Cancer can thin bones for treatment aimed at killing cancerous cells.
Decreased estrogen levels, whether natural or not, can lead to bone thinning in people of all genders. This hormone is often blocked to prevent the spread of estrogen-sensitive tumors.
Your bone density will be monitored during cancer treatment. There are life-style measures that can help protect you from losing bone, and medications that can also help.
If you have osteoporosis and are worried about what a cancer diagnosis might mean, remember that there are medications that can make a difference as well as precautions you can take. Monitoring and treatment for osteoporosis will be part of your care plan.
- On-Site Comments














Comment